Learn more about criteria commonly required by insurance plans for an initial PA for WAKIX and reauthorizations for continued treatment.
Access Prior Authorization Resources
Prior authorization (PA) may be required when prescribing WAKIX
The criteria to obtain coverage for WAKIX will vary among insurance plans. See helpful information below.
For plan-specific coverage, click here.
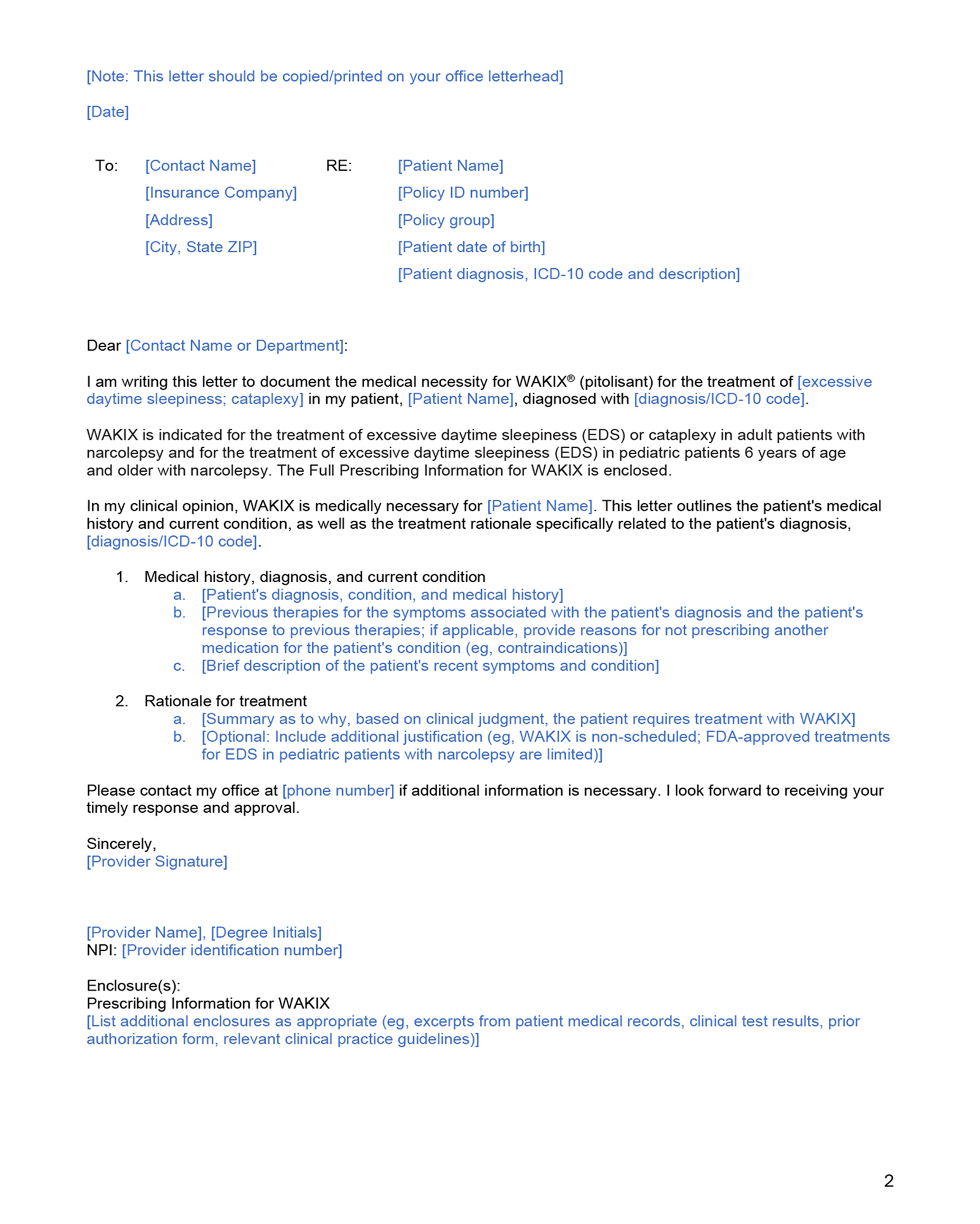
PA brochure

Electronic Prior Authorization (ePA) services are available through CoverMyMeds