American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed, text revision. American Academy of Sleep Medicine; 2023.
Ahmed IM, Thorpy MJ. Clinical evaluation of the patient with excessive sleepiness. In: Thorpy MJ, Billiard M, eds. Sleepiness: Causes, Consequences and Treatment. Cambridge, UK: Cambridge University Press; 2011:36-49.
Pizza F, Filardi M, Moresco M, et al. Excessive daytime sleepiness in narcolepsy and central nervous system hypersomnias. Sleep Breath. 2020;24(2):605-614.
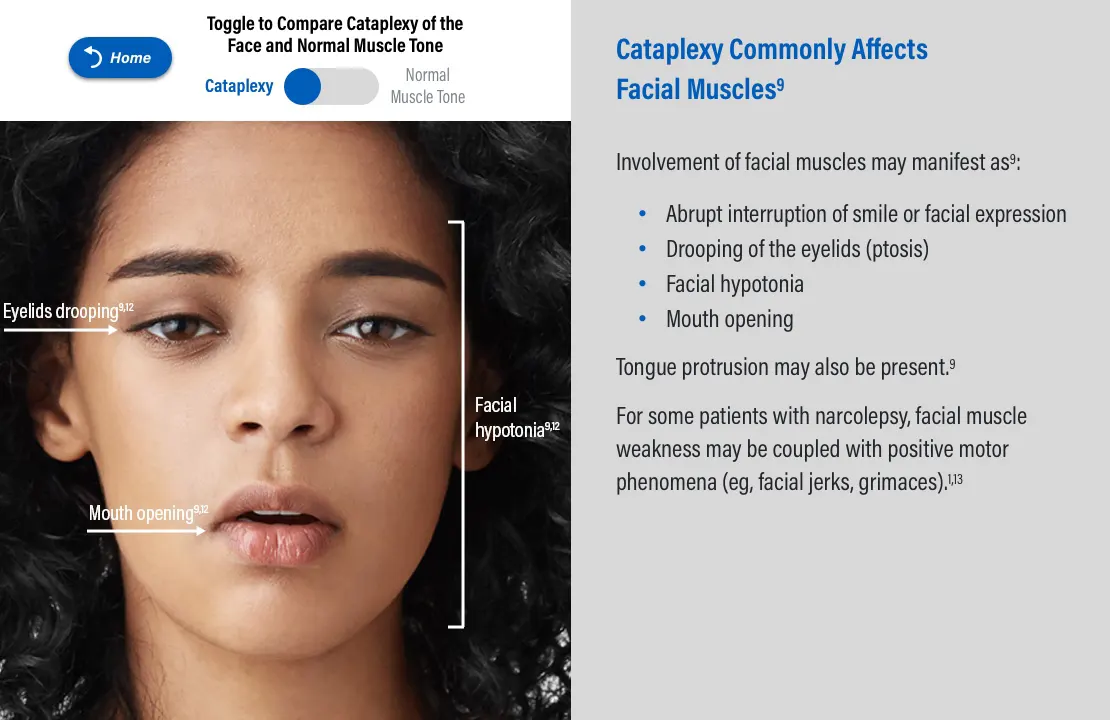
Pizza F, Antelmi E, Vandi S, et al. The distinguishing motor features of cataplexy: a study from video-recorded attacks. Sleep. 2018;41(5). doi:10.1093/sleep/zsy026
Overeem S, van Nues S, van der Zande WL, Donjacour CE, van Mierlo P, Lammers GJ. The clinical features of cataplexy: a questionnaire study in narcolepsy patients with and without hypocretin-1 deficiency. Sleep Med. 2011;12(1):12-18.
Anic-Labat S, Guilleminault C, Kraemer H, Meehan J, Arrigoni J, Mignot E. Validation of a cataplexy questionnaire in 983 sleep-disorder patients. Sleep. 1999;22(1):77-87.
Morse AM. Narcolepsy in children and adults: a guide to improved recognition, diagnosis and management. Med Sci (Basel). 2019;7(12):106. doi:10.3390/medsci7120106
Overeem S. The clinical features of cataplexy. In: Baumann CR, Bassetti CL, Scammell T, eds. Narcolepsy: Pathophysiology, Diagnosis, and Treatment. New York, NY: Springer; 2011:283-290.
Almeneessier AS, Alballa NS, Alsalman BH, Aleissi S, Olaish AH, BaHammam AS. A 10-year longitudinal observational study of cataplexy in a cohort of narcolepsy type 1 patients. Nat Sci Sleep. 2019;11:231-239.
Huang B, Xu T, Wang Z, et al. The clinical characteristics of cataplectic attack in narcolepsy type 1. Sleep Med. 2021;77:261-269.
Sturzenegger C, Bassetti CL. The clinical spectrum of narcolepsy with cataplexy: a reappraisal. J Sleep Res. 2004;13(4):395-406.
Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol. 2018;85:21-32.
Chung I-H, Chin W-C, Huang Y-S, Wang C-H. Pediatric narcolepsy-a practical review. Children (Basel). 2022;9(7):974. doi:10.3390/children9070974
Maski K, Kotagal S. Clinical features and diagnosis of narcolepsy in children. Clinical Decision Support | UpToDate | Wolters Kluwer. Updated July 29, 2024. Accessed September 6, 2024. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-narcolepsy-in-children
Rocca FL, Pizza F, Ricci E, Plazzi G. Narcolepsy during childhood: an update. Neuropediatrics. 2015;46(3):181-198.