Pathophysiology
Narcolepsy Is Characterized by Sleep-Wake State Instability1
During the day, unstable wakefulness can occur as excessive daytime sleepiness (EDS) and cataplexy,1,2 the two most common symptoms of narcolepsy3,4
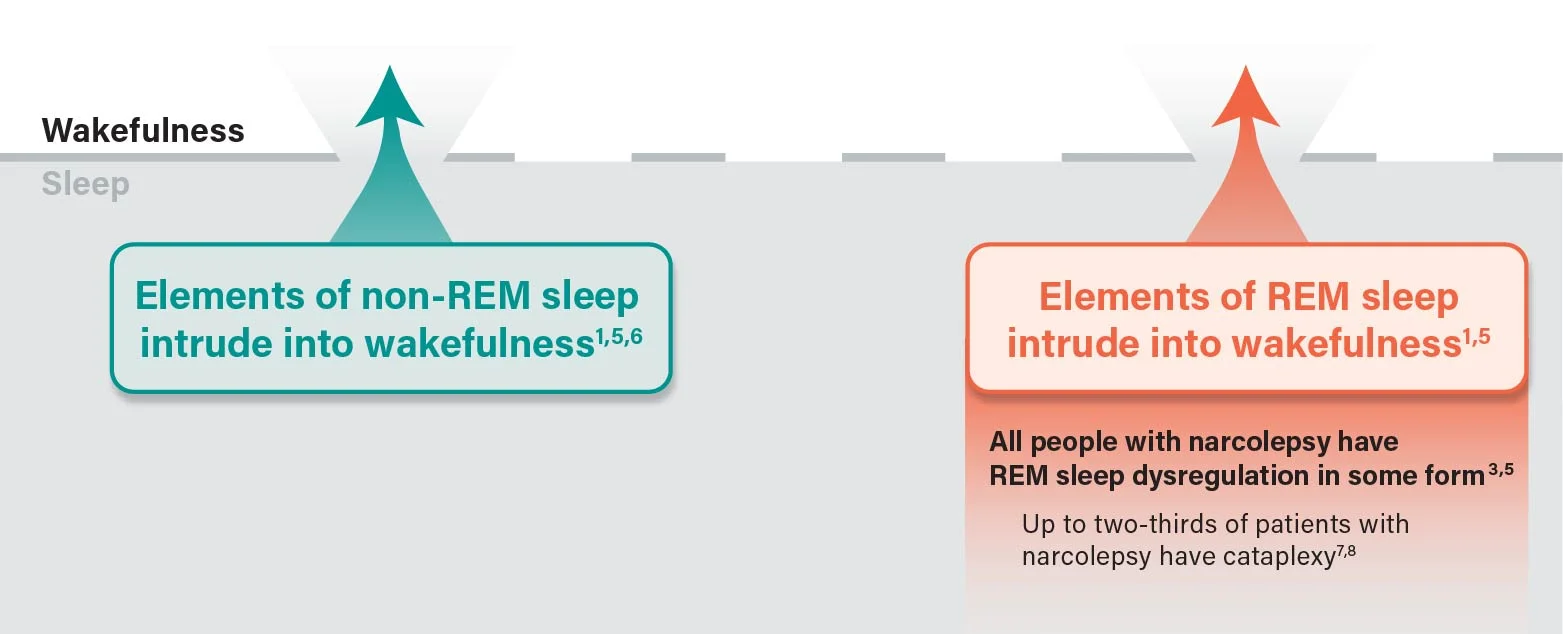
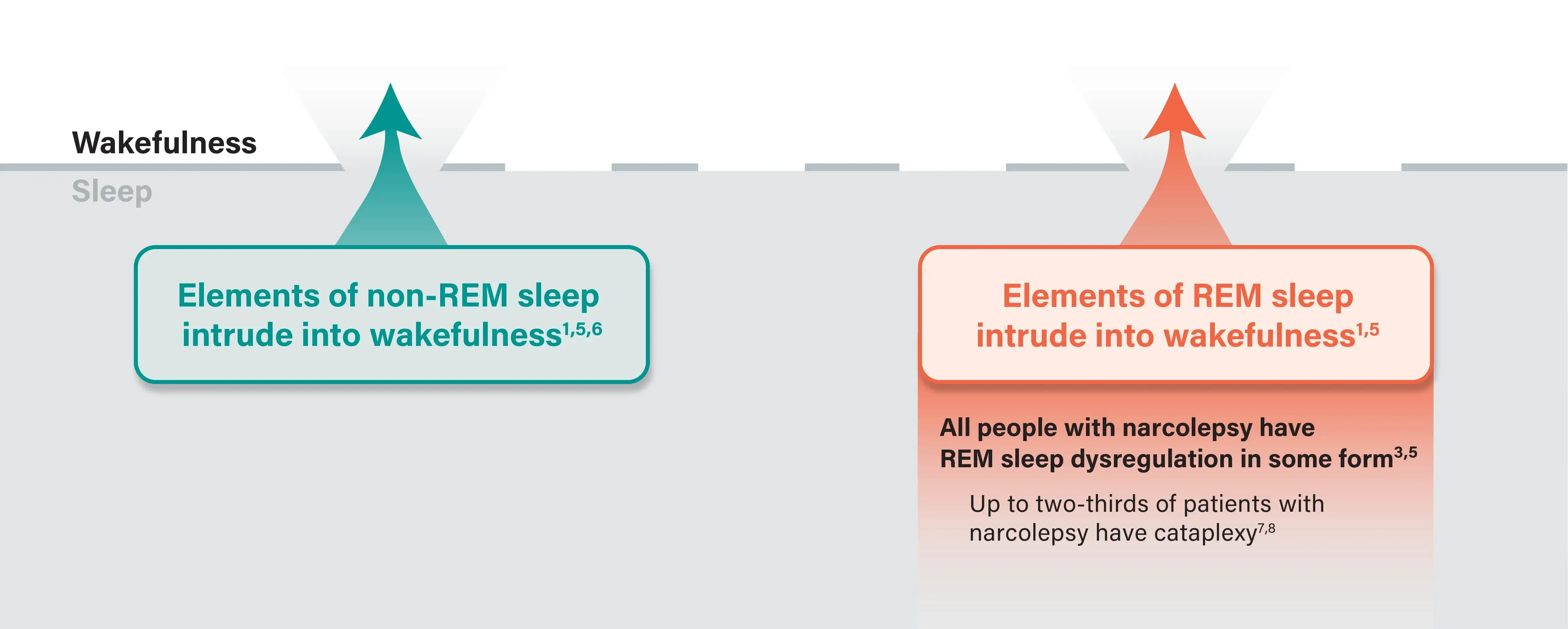
Loss of orexin (hypocretin) neurons in narcolepsy ultimately leads to sleep-wake state instability1,5
- During the day, unstable wakefulness can occur due to:
- Reduced or inconsistent activation of histamine and other wake-promoting neurons1,5
- Periodic activation of REM sleep–promoting neurons and non-REM sleep–promoting neurons1,9,10
Loss of orexin neurons causes narcolepsy in most patients3,7,8
- About 95% of patients with narcolepsy with cataplexy (narcolepsy type 1) are estimated to have low levels of orexin3,*
- 15-20% of patients with narcolepsy without cataplexy (narcolepsy type 2) are estimated to have low levels of orexin† and are more likely to develop cataplexy3
*Low levels of cerebrospinal fluid (CSF) orexin were defined as <110 pg/mL.3
†Low levels of CSF orexin were defined as ≤110 pg/mL.3